Foot Care
Last updated: 09 Sep 2025
Foot problems are a common but often preventable complication for people living with Type 1 Diabetes (T1D), especially as they age. Diabetes can affect the feet in two main ways: by reducing blood circulation (peripheral vascular disease) and by damaging the nerves (peripheral neuropathy).1 This combination means that injuries may not heal well and might not even be felt, potentially leading to serious issues like ulcers and, in severe cases, amputation.2
For older people with T1D, diligent daily foot care and regular professional check-ups are vital to maintaining foot health, mobility, and overall well-being. This page outlines why foot care is so important and provides practical advice on how to look after your feet.
How Diabetes Affects Your Feet
Understanding the impact of diabetes on your feet is the first step towards effective care:
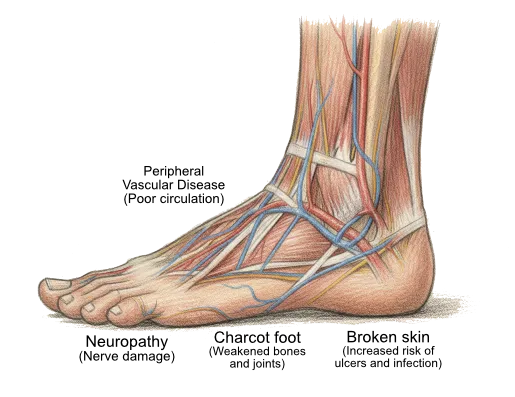
- Nerve Damage (Neuropathy): High blood glucose over time can damage the nerves in your feet.3 This can lead to a loss of sensation, meaning you might not feel pain, heat, cold, or pressure. As a result, minor injuries like cuts, blisters, or stepping on something sharp might go unnoticed and untreated.
- Poor Circulation (Peripheral Vascular Disease): Diabetes can also narrow and harden the arteries that supply blood to your feet and legs.[7] Reduced blood flow means that injuries and infections heal more slowly.[7]
- Increased Risk of Infection: People with diabetes may be more susceptible to infections. An unnoticed and poorly healing injury on the foot can easily become infected.
- Foot Ulcers: A foot ulcer is a break in the skin or a deep sore. They can occur from minor injuries that don’t heal due to poor circulation and lack of sensation. Ulcers require prompt medical attention to prevent serious complications.3
- Charcot Foot: This is a serious condition where bones in the foot weaken and can fracture or dislocate, leading to foot deformity. It can occur in people with significant neuropathy. Signs include a red, hot, swollen foot, possibly with some aching.
Essential Daily Foot Care Routine
A simple daily routine can make a huge difference:
- Inspect Your Feet Daily: Look for any cuts, blisters, redness, swelling, calluses, or changes in skin temperature or colour. Use a mirror if you can’t see the bottom of your feet, or ask a family member or carer to help.
- Wash Your Feet Daily: Use lukewarm water (test the temperature with your elbow, not your foot, if you have neuropathy) and mild soap. Avoid soaking your feet for long periods as this can dry out the skin.
- Dry Your Feet Thoroughly: Pay special attention to drying between your toes to prevent fungal infections.
- Moisturise Dry Skin: Apply a good quality moisturising cream to the tops and bottoms of your feet to keep the skin soft and prevent cracking. Avoid putting cream between your toes.
- Toenail Care:
- Cut toenails straight across and file any sharp edges. Avoid cutting them too short or down the sides, as this can lead to ingrown toenails.
- If you have difficulty seeing, reaching your feet, or have thickened nails, it’s best to have your toenails cut by a podiatrist.
- Never Go Barefoot: Always wear shoes or slippers, even indoors, to protect your feet from injury.3
- Check Inside Your Shoes: Before putting on your shoes, always check inside for any small objects, pebbles, or rough seams that could injure your feet.
Choosing the Right Footwear
Proper footwear is crucial for foot protection:
- Well-Fitting Shoes: Shoes should be comfortable, supportive, and fit well in length, width, and depth. Avoid shoes that are too tight, have pointed toes, or high heels.3 Have your feet measured when buying new shoes, as foot size can change.
- Protective Material: Choose shoes made of breathable materials like leather or canvas.
- Socks: Wear clean, well-fitting socks every day. Socks made from natural fibres (like cotton or wool blends) or moisture-wicking synthetic materials are good choices. Avoid socks with tight elastic tops or prominent seams that could rub.
- Avoid Open-Toed Shoes: Sandals or thongs offer little protection and increase the risk of injury.
When to See a Health Professional
Regular foot checks by a healthcare professional are essential:
- Annual Foot Check: Everyone with diabetes should have a comprehensive foot examination by a doctor, podiatrist, or credentialed diabetes educator at least once a year. This check assesses your circulation, nerve sensation, and overall foot health to determine your risk of foot problems.
- More Frequent Checks if High Risk: If you have existing foot problems, neuropathy, poor circulation, or a history of ulcers, you will need more frequent checks by a podiatrist.
- Urgent Attention for New Problems: Seek immediate advice from your doctor or podiatrist if you notice any of the following 4:
- A cut, blister, sore, or ulcer that isn’t healing or looks infected (red, swollen, warm, pus).
- Pain, throbbing, heat, or swelling in your foot.
- Changes in the colour or shape of your foot.
- Numbness, tingling, or unusual sensations.
- Signs of a suspected Charcot foot (unilateral red, hot, swollen, possibly aching foot).
Do not attempt to treat corns, calluses, or ingrown toenails yourself, especially if you have neuropathy or poor circulation. Always see a podiatrist.
Key Takeaways
- Diabetes can damage nerves and reduce blood flow to the feet, increasing the risk of serious foot problems.2
- Daily foot inspection and care, along with wearing appropriate footwear, are crucial for prevention.
- Regular professional foot checks (at least annually) are essential for early detection and management of potential issues.
- Seek urgent medical attention for any new foot injury, infection, or concerning changes.4
Where to Get Help
- Your GP (Doctor): For initial assessment, referrals, and managing overall diabetes care.
- Podiatrist: Experts in foot care. You don’t always need a referral, but your GP can provide one, potentially under a Chronic Disease Management Plan which may allow for Medicare rebates for some allied health services.
- Credentialed Diabetes Educator (CDE): Can provide education on foot care as part of overall diabetes self-management.
- Diabetes Victoria: Offers information and resources on foot care. Tel. 1300 437 386.
- National Diabetes Services Scheme (NDSS): Provides information and support. Tel. 1800 637 700.
- High-Risk Foot Services: Specialised clinics for complex foot problems, often located in hospitals. Your GP or podiatrist can refer you if needed.
- Baker Heart and Diabetes Institute Diabetes Clinic: Tel. (03) 8532 1800.